Have you noticed stubborn belly fat that won’t budge despite eating well and exercising regularly? You might be dealing with stress belly, not regular fat accumulation. Understanding the difference between stress-induced belly fat and typical fat storage can transform your approach to weight loss and health.
Stress belly, often called cortisol belly, develops through entirely different mechanisms than regular fat gain. While traditional belly fat responds to calorie reduction and physical activity, stress belly requires a fundamentally different approach focused on hormonal balance and nervous system regulation.
What Is Stress Belly and How Does It Form?
Stress belly refers to abdominal fat accumulation triggered by chronically elevated cortisol levels. When your body experiences ongoing stress, whether from work pressure, relationship challenges, financial worries, or lack of sleep, it releases cortisol as part of the stress response system.
Unlike regular fat that accumulates gradually from excess calorie consumption, stress belly develops as a protective mechanism. Your body interprets chronic stress as a survival threat and responds by storing energy reserves in the most accessible location: your midsection.
Cortisol & Central Fat Storage: The Hormonal Connection
Cortisol doesn’t just make you “gain weight”; it specifically dictates where that weight goes. Here is the hormonal science behind why your midsection is the primary target:
- The “Stress Eating” Signal: Cortisol triggers cravings for “hyper-palatable” foods—those high in sugar and fat. This is an evolutionary survival tactic designed to provide quick energy for a “fight or flight” response.
- Abdominal Receptor Density: Research shows that visceral fat tissue (the fat deep in your belly) has significantly more cortisol receptors than fat in your hips or thighs. This makes your midsection a “magnet” for fat storage whenever cortisol levels are high.
- The Insulin Resistance Loop: Chronic cortisol elevation forces the liver to release glucose for extra energy. This causes insulin levels to spike. Over time, this leads to insulin resistance, a state where your body becomes incredibly efficient at storing fat and almost incapable of burning it.
- Hormonal Suppression: High cortisol acts like a “bully” to other hormones. It suppresses thyroid-stimulating hormone (slowing metabolism) and reduces growth hormone and testosterone, leading to muscle loss and further fat accumulation.
Why Stress Belly Keeps Growing Even When You’re Dieting
One important reason stress belly is so stubborn lies in a special enzyme found in deep belly fat called 11β-HSD1. This enzyme converts inactive cortisol into active cortisol right inside the belly fat itself.
Even if your stress levels or blood cortisol are not very high, visceral belly fat can make its own cortisol locally. This creates a vicious cycle:
- Stress increases cortisol production.
- Cortisol encourages belly fat storage.
- Belly fat produces more cortisol via 11β-HSD1.
- More cortisol leads to even more belly fat.
Because of this loop, stress belly often does not respond to dieting alone. Eating less may reduce calories, but it does not stop this local cortisol production, which is why the belly area remains stubborn.
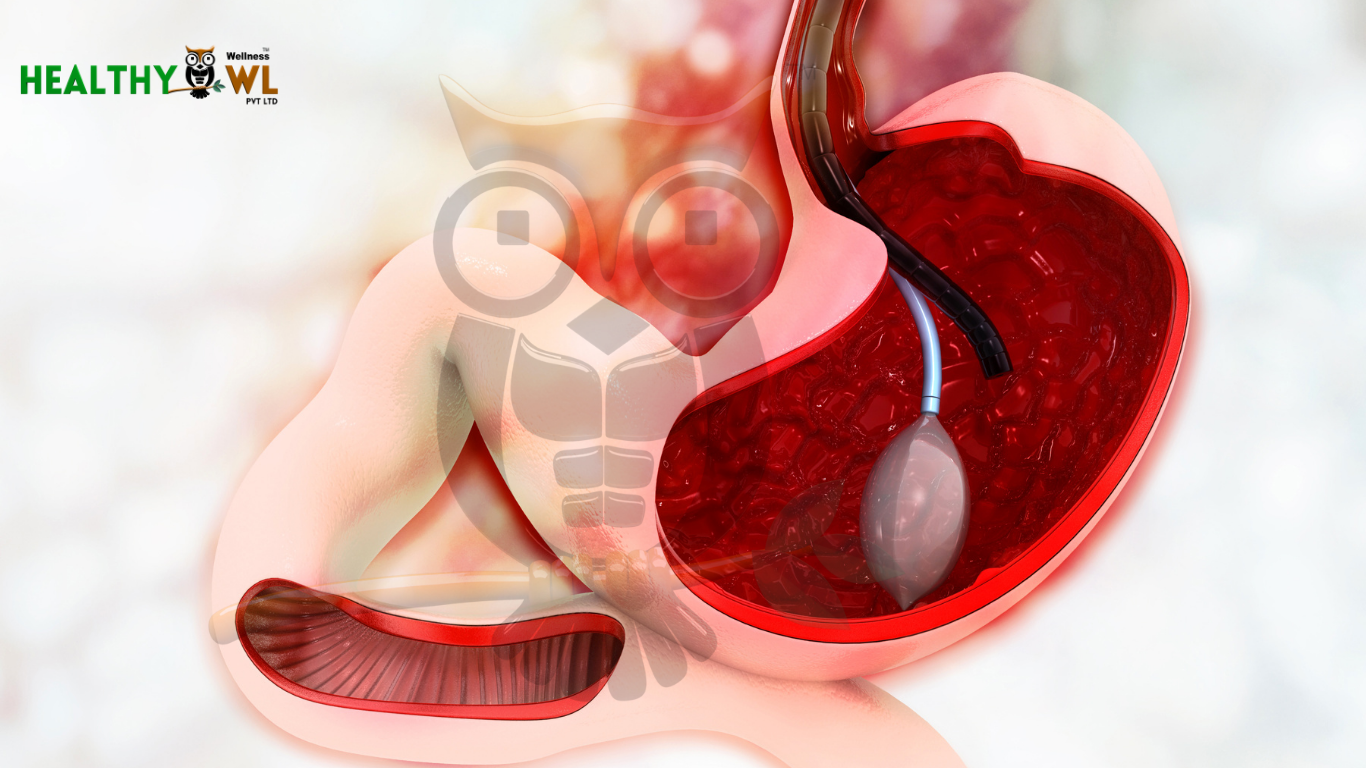
Visceral Fat vs Subcutaneous Fat: Understanding the Dangerous Difference
Not all belly fat is created equal. The distinction between visceral and subcutaneous fat explains why stress belly is deeper, harder, and metabolically more dangerous.
- Subcutaneous Fat: Sits just beneath the skin surface. You can pinch this fat between your fingers. While excess subcutaneous fat affects appearance, it is relatively metabolically inert.
- Visceral Fat (Stress Belly): Surrounds your internal organs deep within the abdominal cavity. You cannot pinch visceral fat. It wraps around your liver, pancreas, and intestines.
Visceral fat is metabolically active tissue that functions like an endocrine organ, releasing inflammatory compounds called cytokines. This contributes to systemic inflammation and increases the risk of serious health conditions.
How Stress Belly Connects to Other Health Conditions
| Condition | How It Connects to Stress Belly |
| Hypothyroidism | Elevated cortisol suppresses thyroid hormones, slowing metabolism and promoting fat storage. |
| PCOD / Insulin Resistance | Cortisol worsens insulin resistance, increasing abdominal fat deposition. |
| Poor Gut Health | Chronic stress alters gut bacteria and increases inflammation, contributing to bloating. |
| Sleep Disorders | Inadequate sleep keeps cortisol elevated, preventing visceral fat loss. |
| Chronic Inflammation | Visceral fat releases inflammatory markers, creating a self-perpetuating stress loop. |
Key Differences Between Stress Belly and Regular Fat Belly
Distribution Pattern
Stress belly typically presents as a round, protruding abdomen that seems disproportionate to the rest of the body. People with a stress belly may have relatively slim arms and legs but carry significant weight around their midsection. Regular fat gain tends to distribute more evenly across the body, including the hips, thighs, arms, and face.
Texture and Feel
Stress belly feels firm and tight because visceral fat packs densely around organs. Regular belly fat usually feels softer and more movable because subcutaneous fat has room to expand beneath the skin.
Response to Diet and Exercise
Traditional fat responds predictably to calorie deficit and increased physical activity. Stress belly, however, can be stubbornly resistant to conventional weight loss methods if cortisol levels remain elevated.
Associated Symptoms
Stress belly often accompanies other signs of chronic stress and cortisol dysregulation, including disrupted sleep, constant fatigue, sugar cravings, mood swings, anxiety, difficulty concentrating, and reduced immunity. Regular weight gain typically doesn’t present with these specific symptom clusters.
Health Risks
While all excess body fat carries some health risks, visceral fat associated with stress belly poses significantly greater dangers. The inflammatory and metabolic effects of visceral fat create a higher risk for serious conditions compared to equivalent amounts of subcutaneous fat.
Distribution Pattern
Stress belly typically presents as a round, protruding abdomen that seems disproportionate to the rest of the body. People with stress belly may have relatively slim arms and legs but carry significant weight around their midsection. Regular fat gain tends to distribute more evenly across the body, including hips, thighs, arms, and face.
Texture and Feel
Stress belly feels firm and tight because visceral fat packs densely around organs. Regular belly fat usually feels softer and more movable because subcutaneous fat has room to expand beneath the skin.
Response to Diet and Exercise
Traditional fat responds predictably to calorie deficit and increased physical activity. Stress belly, however, can be stubbornly resistant to conventional weight loss methods if cortisol levels remain elevated.
Associated Symptoms
Stress belly often accompanies other signs of chronic stress and cortisol dysregulation, including disrupted sleep, constant fatigue, sugar cravings, mood swings, anxiety, difficulty concentrating, and reduced immunity. Regular weight gain typically doesn’t present with these specific symptom clusters.
Health Risks
While all excess body fat carries some health risks, visceral fat associated with stress belly poses significantly greater dangers. The inflammatory and metabolic effects of visceral fat create a higher risk for serious conditions compared to equivalent amounts of subcutaneous fat.
Why Diet & Exercise Alone Don’t Reduce Stress Belly
Many people become frustrated when calorie restriction and exercise fail to reduce their stress belly. The explanation lies in understanding that stress belly is fundamentally a hormonal issue, not simply an energy balance problem.
When you diet while cortisol remains elevated, you create additional stress on your body. Caloric restriction signals potential famine, triggering more cortisol release as a survival response. This counterproductive cycle can actually worsen stress belly despite your best dietary efforts.
Similarly, excessive exercise, particularly high-intensity training without adequate recovery, elevates cortisol levels. While moderate physical activity helps reduce stress, overtraining adds physical stress that compounds the problem. This explains why marathon runners and intense fitness enthusiasts sometimes develop stress belly despite high activity levels.
The Missing Role of Sleep in Stress Belly Reduction
Sleep deprivation ranks among the most powerful drivers of cortisol elevation and stress belly development. Even one night of poor sleep significantly raises cortisol levels the following day. Chronic sleep restriction creates a state of physiological stress that promotes visceral fat accumulation.
During deep sleep, cortisol levels naturally drop to their lowest point, allowing your body to recover and repair. When sleep is insufficient or fragmented, cortisol never fully decreases, maintaining elevated levels around the clock.
Research consistently shows that people sleeping less than seven hours nightly have higher rates of abdominal obesity compared to those getting adequate rest. Prioritizing seven to nine hours of quality sleep becomes essential for reducing stress belly.
Nervous System Recovery: The Foundation of Cortisol Regulation
Your autonomic nervous system operates in two modes: sympathetic (fight-or-flight) and parasympathetic (rest-and-digest). Chronic stress keeps you locked in sympathetic dominance, with constantly elevated cortisol and adrenaline.
Reducing stress belly requires actively shifting toward parasympathetic activation through specific practices. Deep breathing exercises, meditation, gentle yoga, nature exposure, and social connection all stimulate the vagus nerve and promote parasympathetic activity.
Many people unknowingly maintain sympathetic dominance throughout their day through constant digital stimulation, multitasking, caffeine consumption, and lack of genuine rest periods. Building regular nervous system recovery into your daily routine becomes as important as diet and exercise for addressing stress belly.
Cortisol Regulation: Beyond Stress Management
While stress management matters, cortisol regulation requires attention to multiple factors beyond mental stress. Blood sugar instability, chronic inflammation, gut dysfunction, nutrient deficiencies, and circadian rhythm disruption all affect cortisol patterns.
Eating balanced meals with adequate protein and healthy fats stabilizes blood sugar and prevents cortisol spikes. Reducing inflammatory foods while increasing anti-inflammatory nutrients supports healthier cortisol rhythms. Healing gut issues and maintaining circadian alignment through consistent sleep-wake times and morning light exposure further optimizes cortisol regulation.
How to Address Stress Belly: A Comprehensive Approach
Successfully reducing stress belly requires a multi-faceted strategy addressing the root causes of cortisol elevation:
Prioritize sleep quality and quantity as your foundation. Create a consistent sleep schedule, optimize your bedroom environment, and address any sleep disorders.
Practice daily stress reduction techniques, including meditation, deep breathing, progressive muscle relaxation, or mindfulness exercises, for at least 10-15 minutes.
Balance your exercise routine with moderate-intensity activities, such as walking, swimming, or cycling, while avoiding overtraining. Include restorative practices, such as yoga or tai chi.
Stabilize blood sugar by eating protein-rich meals, reducing refined carbohydrates and sugars, and avoiding long periods without food.
Support your gut health through probiotic-rich foods, adequate fiber, and reducing inflammatory foods that may trigger stress responses.
Build recovery periods into your day with breaks from screens, time in nature, social connection, and activities that genuinely relax you.
Consider cortisol-supporting nutrients, including vitamin C, magnesium, omega-3 fatty acids, and adaptogenic herbs like ashwagandha (consult with a healthcare provider).
Address underlying stressors where possible through boundary-setting, time management, professional support, or lifestyle changes.
What Not to Do If You Have Stress Belly
When people realize they have a “stress belly,” they often double down on the wrong habits, which actually spikes cortisol further. Avoid these common mistakes:
- Extreme Caloric Restriction: Cutting calories too low signals a “famine” to your brain, causing the body to cling to fat for survival.
- Excessive High-Intensity Cardio: Overtraining without recovery keeps your body in a state of “sympathetic dominance” (fight or flight), preventing fat burning.
- Relying on Caffeine to Get Through the Day: Caffeine stimulates the adrenal glands. If you are already stressed, excess coffee is like pouring gasoline on a fire.
- Sacrificing Sleep for the Gym: Sleep is when cortisol resets. Choosing a 5 AM workout over a necessary extra hour of sleep can actually prevent you from losing belly fat.
Frequently Asked Questions
Q- What does a stress belly look like?
It typically presents as a round, firm, protruding abdomen. Unlike a “spare tire” that hangs over the belt, a stress belly feels tight because the fat is pushing outward from behind the abdominal muscles
Q- How do I know if I have stress belly or regular fat?
If your weight gain is concentrated solely in the abdomen while your arms and legs remain thin, and if it is accompanied by “tired but wired” feelings at night, sugar cravings, and brain fog, it is likely cortisol-driven
Q- Can you lose stress belly without reducing stress?
Losing stress belly without addressing underlying stress proves extremely difficult because elevated cortisol actively promotes visceral fat storage. While diet and exercise contribute to overall health, sustainable stress belly reduction requires cortisol regulation through improved sleep, stress management practices, nervous system recovery, and hormonal balance.
Q- How long does it take to lose stress belly?
Hormonal changes take time. While you might feel better within a week of improving sleep and stress management, physical changes in visceral fat usually take 4 to 8 weeks of consistency to become visible.
Q- What foods reduce cortisol and stress belly?
Foods that help reduce cortisol and stress belly include fatty fish rich in omega-3s, dark leafy greens, berries high in antioxidants, nuts and seeds providing magnesium, probiotic foods like yogurt and kefir, green tea, dark chocolate, and foods rich in vitamin C. Equally important is avoiding excessive caffeine, alcohol, refined sugars, and processed foods that can spike cortisol levels.
Q- Does drinking water help with stress belly?
Proper hydration supports cortisol regulation and overall metabolism, making it helpful for reducing stress belly. Dehydration creates physical stress that raises cortisol levels. Drinking adequate water throughout the day, particularly first thing in the morning, helps maintain optimal hormonal balance and supports your body’s natural detoxification processes.
Conclusion: A New Approach to Stubborn Belly Fat
Understanding that stress belly differs fundamentally from regular fat empowers you to take the right approach. While conventional weight loss focuses on calories and exercise, reducing stress belly requires addressing the hormonal and physiological roots of cortisol elevation.
By prioritizing sleep, managing stress effectively, supporting your nervous system, and regulating cortisol through comprehensive lifestyle changes, you can successfully reduce a stubborn stress belly. This approach not only transforms your appearance but also significantly improves your metabolic health, reducing risk for serious chronic diseases associated with visceral fat accumulation.
Remember that stress belly developed over time and will require patience and consistency to resolve. Focus on progress rather than perfection, celebrating small improvements in energy, sleep quality, and stress levels as indicators you’re moving in the right direction. Your body has a remarkable healing capacity when given the proper support to restore hormonal balance and metabolic health.
Ready to take control of your stress belly? Visit Healthy Owl Wellness for personalized guidance on cortisol regulation, stress management, and sustainable wellness solutions tailored to your unique needs.